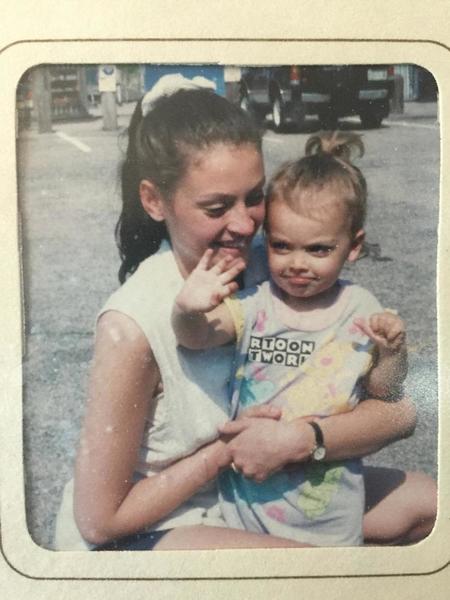
Heidi Aylward spent much of 2015 going to doctor’s appointments for back and joint pain, dizziness, swelling of the legs and feet, high blood pressure, elevated platelets, heart palpitations and extreme fatigue.
2016 isn’t looking much better. She’s worn a heart monitor, had a bone marrow biopsy and continues to have blood work. She holds down a job as a full-time project manager, tends to her daughters, home and pets.
But she feels like her body is falling apart.
“I’m not going to make it to 60,” she said, “Why do I even contribute to my retirement savings account?”
Heidi is 39.
She’s also one of my best friends.
I can’t help but wonder how much her body is burdened by her chaotic childhood.
For personal and professional reasons, I’ve been learning about the new science of human development, which includes the epidemiology of childhood adversity and how toxic stress from childhood trauma can damage the structure and function of a child’s developing brain. Toxic stress also embeds in a person’s biology to emerge decades later as physical disease.
The CDC-Kaiser Permanente Adverse Childhood Experiences Study (ACE Study) shows that childhood trauma is linked to the adult onset of chronic disease, mental illness, violence and being a victim of violence. The research, led by Dr. Vincent Felitti (Kaiser) and Dr. Robert Anda (CDC) measured 10 types of childhood adversity that occurred before the age of 18.
They are physical (1), verbal (2) and sexual abuse (3); physical (4) and emotional (5) neglect; a family member who has been incarcerated (6), is abusing alcohol or drugs (7), or has a mental illness (8), witnessing a mother being abused (9); and losing a parent to divorce or separation (10). The lowest possible score is 0 and the highest 10. Of course there are many other types of childhood adversity – bullying, witnessing violence outside the home, being homeless, witnessing a sibling being abuse, experiencing a severe illness or accident – but this study focused just on these 10.
The higher a person’s ACE score, the greater the risk of chronic disease and mental illness. For example, compared with someone who has an ACE score of zero, a person with an ACE score of 4 or more is twice as likely to have heart disease, seven times more likely to be alcoholic and 12 times more likely to attempt suicide. Of the 17,000 mostly white, college-educated people with jobs and great health care who participated in the study, 64 percent had an ACE score of 1 or more; 40 percent had 2 or more and 12 percent had an ACE score of 4 or more (i.e., four out of the 10 different types of adversity).
Adverse childhood experiences (ACEs) contribute to most of our major chronic health, mental health, economic health and social health issues.
Heidi and I were both diagnosed with PTSD in our 20’s. Combined, we’ve seen our share of therapists, doctors, nurse practitioners, social workers, psychiatrists and healers. We’ve discussed how childhood chaos contributes to lousy moods or relationships, but never poor health, disease, discomfort or premature aging or dying early.
Not one medical professional had talked to either one of us about ACEs or mentioned how early adversity poses health risks and concerns.
In fact, when Heidi asked her doctor about the ACE Study at her appointment, he told her:
“There’s a school of thought that says it’s better not to bring up the past or think about it.” She felt defeated and irked.
“It’s not so much that I was thinking about the past a lot,” she says, “it’s just the way my body reacts to stress.” She thought it might be relevant.
She’s not wrong.
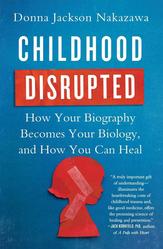
“Hundreds of studies have shown that childhood adversity hurts our mental and physical health, putting us at greater risk for learning disorders, cardiovascular disease, autoimmune disease, depression, obesity, suicide, substance abuse, failed relationships, violence, poor parenting, and early death,” writes Donna Jackson Nakazawa in Childhood Disrupted: How Your Biography Becomes Your Biology and How You Can Heal.
Dr. Jeffrey Brenner, recipient of a 2013 MacArthur Foundation genius award, wrote: “ACE Scores should become a vital sign, as important as height, weight, and blood pressure.”
But they aren’t. Not yet.
“We’re on the cusp of a sea change,” said Jackson Nakazawa, “I don’t think it can happen fast enough.”
She pointed to the nascent ACEs movement, which keeps her optimistic.
There are nearly 10,000 members of ACEsConnection.com, a social network for people who are implementing trauma-informed and resilience-building practices based on ACEs science.
Supporting her optimism for change is the fact that hospitals now have birthing centers and integrative medicine approaches, both of which happened relatively quickly. Neither were “driven by physicians,” she said, but “by patients – and hospital centers realizing they were losing a lot of business” as people left and were willing to travel to birthing clinics or places with integrative approaches.”
As I did.
Motivated entirely by the ACE Study -- particularly the statistic about those with an ACE score of 6 who die decades earlier than those with an ACE score of zero -- I drove almost an hour out of my way to meet a nurse practitioner in a functional medicine practice.
As a result, I had the single best medical appointment of my life.
It was in October 2014, and it was a one-hour conversation I had with Lisa Vasile, a nurse practitioner of functional medicine at Visions Healthcare in Needham, MA.
We sat by her desk.
She didn’t poke or prod my body. She didn’t record my weight, height or blood pressure. She didn’t wear a lab coat or ask me to be naked under a johnnie. We talked.
I told her I wasn’t sleeping well and was hoping to taper off medications for post-traumatic stress disorder. I was weighing the long-term side effects of prescription drugs with the possible relapse or withdrawal if I went off. My concerns were early menopause, premature aging and worries about disease and early death.
I brought a research binder about the ACE Study from the Centers for Disease Control and Prevention (CDC) website.
“We know stress is a major player in disease, (stress) happening now or in childhood where it’s been cumulative,” she said, which is why functional medicine practitioners, “dive deep” into childhood.
Unlike traditional medicine, which often focuses on the treatment of acute problems, often with drugs and surgery, functional medicine explores the causes of diseases and issues. Patients partner with practitioners to identify, treat and prevent them, and start their journey with a practitioner who takes a thorough history.
“Were you a wanted child?” was one of the first questions Vasile asked me.
“It’s probably safe to say I wasn’t planned,” I said.
I told her my mother got pregnant at 16 with my sister, and was 19 when she had me. I told her I didn’t know my father, a violent alcoholic who left before my first birthday.
She wasn’t looking for fill-in-the blank answers. She made eye contact with me and was curious about my experience of my own childhood. That felt so different than being with someone filling out a form or staring from behind a computer screen.
We went over falls -- one from a porch and another from a moving car -- and the pinky that got amputated before I was two. I mentioned abuse, bed-wetting and when my period started, as well as family moves and changing dads, towns and schools.
She treated trauma and family facts the same as information about ear infections, bronchitis and antibiotic use. She seemed neutral, caring and curious.
At typical appointments, when asked about my father’s health, I have said “unknown,” if I feared the person asking would be unable to handle hearing about homelessness, alcoholism, abuse, desertion or mental illness without judging me. Psych topics often feel out of place with physicians, like ordering steak off a vegan menu.
Vasile was different, even in the way she worded things, such as when she asked:
“How did those early childhood experiences manifest during the teens?”
How - not if.
It made it easier to mention depression, migraines, anemia and my use of diet pills.
It made it possible to share a secret I’d never disclosed with a nurse or doctor – that I’d been bulimic for most of my teens. In every other medical appointment, I had held back this information even when I’d had a spastic colon, GI problems, vitamin deficiencies and problems absorbing food as an adult. It was embarrassing, long in the past and no one had ever asked.
Vasile asked everything about my childhood, including if I did sports, had friends and what skills and passions I’d had.
She seemed to break my childhood into four distinct periods.
1. 0-5
2. 6-12
3. 13-18
4. 19-24
I’m not sure I’d ever talked about the college years, which had been particularly rough for me. Even though I was the first in my family to finish college. I did not feel lucky. During those years, my grandmother and the guy I called Dad both battled cancer and died. My sister met our biological father, and a friend committed suicide. I got anxiety attacks for the first time and was diagnosed with post-traumatic stress disorder (PTSD) by the therapist I started seeing.
Nothing I said seemed to shock Vasile. She just nodded her head as if I’d say my skin was itchy after the chicken pox.
She even educated me about the impact of stress:
• how stress in childhood prevents proper growth and the way the body handles stress;
• how frequent antibiotic use from ear infections or bronchitis can impact gut health and weaken the immune system;
• how nutrition can be used to support good health;
• how an eating disorder, vegetarianism and anemia, all of which I had during my teens, can contribute to depression and anxiety;
• how my childhood and adult stressors probably had an influence on the age I was when menopause started.
She explained the tests she’d like to have done.
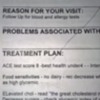
• Blood work to check my hormones, vitamins, minerals, cholesterol;
• Blood work to assess cardiac health and inflammation;
• A bone scan to check bone health as bulimia can be a factor in osteoporosis;
• The mammogram I was behind on;
• Allergy testing.
As for tapering off prescription medications for PTSD, she suggested waiting on test results. She didn’t want to place any additional demands on me such as weaning off medications without supporting me better first.
I teared up in relief. I confessed that even though my PTSD management skills were strong, life had been harder since menopause. I felt more fragile, less hearty and didn’t know if it was from hormone changes or life events (divorce, flood, money, mid-life dating).
I’d always been able to dig deep, into my bone marrow if necessary, to suck it up, endure or rally but this ‘super power’ seemed to be fading fast. I wondered if my nervous system was like a set of balding tires that I couldn’t replace or change. I’d hydroplane and skid off course easily no matter how slowly I drove. Could I get some tread back in order to cover more varied terrain without worry about flat tires?
After our visit, I made more sense to myself. My symptoms weren’t strange. I wasn’t strange. Vasile thought there were things she could suggest which might provide some relief.
She validated my concerns and experiences. Rather than leave feeling numb, depressed or like damaged goods, the way I usually felt leaving medical appointments, I felt great.
She treated me like a marathon runner at the end of a race – as though I was successful but tired. She was there with a high five, water and a blanket.
It was life-changing.
Jackson Nakazawa said others have benefitted from ACE-informed medical appointments. She wrote:
“In one recent study of 125,000 patients, Felitti found that those who took the ACE Study questionnaire as part of their medical history and who discussed their ACE Scores with their doctors had a 35% reduction in their doctor visits and an 11 percent reduction in emergency room visits over the course of the following year.”
Why?
The “practitioner-patient conversation is a really important conversation,” said Jackson Nakazawa. “When the doctor is fully present and caring, we begin to activate reward mechanisms in the brain that are associated with a healing effect, similar to the placebo response.” When we activate “this interpersonal neurobiology between patient and doctor, the relationship becomes a healing force that furthers personal healing,” she said.
Is it possible that some people would just avoid going to doctors and hospitals after an ACE conversation because it's awkward or painful to talk about the past? I can't speak for others but that wasn’t the case for me. It was a relief not to suppress, deny or avoid the truth of trauma or complicated family stories or medical background.
I know I felt better about my past, future and myself after my appointment.
I couldn’t wait for my follow-up where my test results would be discussed and we’d develop my personalized don’t-die-early plan.
The Don’t-Die-Early-Plan to Combat My High ACE Score
My grandfathers both died at about age 50. One of a heart attack and one from cirrhosis. My paternal grandmother died of cirrhosis in her later 50’s and my maternal grandmother died of cancer in her mid-60’s. My mother battled cancer in her early 20’s – and twice in recent decades. Alcoholism and mental illness plagued my father starting in his teens and until he died of cirrhosis at age 69.
Gone is the smug notion that as long as I don’t drink or smoke I can be a doting grandmother living well into my 90’s. Being a sober non-smoker doesn’t inoculate me from health risks associated with developmental trauma and post-traumatic stress. There’s no easy way to override the long reach of childhood toxic stress, trauma and neglect.
Is it possible for me to live a normal life span?
Can I reverse the death-disease-despair curse of early adversity?
“There is no recipe or formula” for those with high ACE scores, says Vasile. “Everybody is different and every BODY is different.”
However, Vasile’s approach to health that she uses with all her patients is one that I’ve found helpful. It’s called DINE.
D is for Detox.
I is for Inflammation.
N is for Nutrition.
E is for Energy.
Detox
Detox involves removing health threats such as smoking cigarettes, drug or alcohol abuse, and even food, which many people use food as medicine or a coping mechanism, she says, either to numb or comfort themselves.
Vasile advises most of her patients to limit or eliminate dairy and gluten from the diet, no matter whether they’re allergic or not. Doing so, will “reduce inflammation in the body” and “makes people feel better” because “the immune system and serotonin levels get shot because of dairy or gluten,” she says. She suggests “eating as many colors of fresh fruit and vegetables in the rainbow as possible.”
She addressed unhealthy relationships with other people, jobs, situations or environments as part of her detox approach as well. It helped me admit how stressful it had become to live in a flood zone as sea levels raise.
Some changes, like moving, cause more stress before things improve and this can be more challenging when changing or leaving jobs or relationships too.
Inflammation
“We know stress is bad” and “crucial in disease,” Vasile explains, “Cumulatively - it’s worse.”
“Stress is fine if you’re running from a tiger,” she explains, but stress “isn’t curative. It’s inflammatory. It inflames and attacks the body.”
She explains how not sleeping well, one of my menopausal problems, can “increase cortisol and cortisol being up all the time is very inflammatory on the body. “
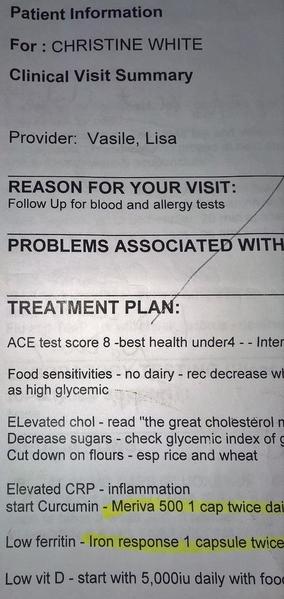
She says studies have shown C-reactive protein (CRP) increases after major life stressors. To assess cardiac health and inflammation, she tested my CRP level.
My CRP was elevated, which didn’t surprise her given my childhood adversity and major adult stressors such as divorce, single parenting and having my home flood twice. She recommended an anti-inflammatory, and to “make yourself happy on a regular basis.”
Daily joy might mean meditation for some or painting the toe nails for others. She sometimes recommends acupuncture and Reiki in addition to anti-inflammatory supplements for those with high CRP levels.
Nutrition
For good nutrition, Vasile had one simple bit of advice: “Eat as many foods with a sticker UPC code on them -- like apples and peppers have -- as possible.” The suggestion many of us hear -- to shop the perimeters of grocery stores where food is fresh -- is ideal.
For me, she suggested Vitamin D supplements at a high dose (5000 iu daily with food), magnesium (in powder form, at night, 175 to 350 mg. daily) and iron (with organic beet root, twice a day with Vitamin C) as my levels were all low. The magnesium was meant to improve my sleep and reduce my anxiety.
She suggested daily fish oil supplements as well as primrose oil. I got only the fish oil only (to save money).
Energy
By energy, Vasile means moving energy with exercise and physical activity, as well as working with the energy system as is done with techniques such as acupuncture, body work and with spirituality.
She calls energy the “fourth leg of a healthy table” that stabilizes the system so it’s less likely to tip. The types of energy work she’s recommended for people to use at home are meditation, journaling, HeartMath, (a type of biofeedback which can be done online or on smart phone 5 to 10 minutes a day), as well as walking and yoga.
Journaling, hypnotherapy, therapy, and EMDR are ways she suggests to help balance energy after trauma, she said. “Any way to pull (trauma) out and dump it instead of carrying it” in the body can be useful.
She suggests a daily gratitude list or journal before bed so people are “shutting down with the positive” each night. This practice can increase levels of happiness in three to six months.
“There’s a lot of research that journaling is very therapeutic,” she also said. She suggests a three-page writing habit each morning with page one used to dump stress, page two listing things to look forward to and the third page detailing what one is thankful for.
I’ve written in my journal since I was 11, and she encouraged me to continue. We pondered whether writing might be one reason my health is not worse.
I had two appointments within three months with Vasile - enough to make me feel empowered and hopeful about my physical and emotional health. However, the practice that employed her, Visions Healthcare, closed in August 2015 soon after implementing a $33 per month fee for patients. Because insurance companies only covered a fraction of most office visits, the patient payment plan was meant to help defray costs. Patients such as myself were unwilling or unable to pay. Vasile runs a private practice now, 4 Better Health, in Hopkinton, MA.
While I can no longer afford to see Vasile at her new practice, I’ve benefited from my two insurance-covered appointments. I’m incorporating her DINE protocol with some success.
• DETOX -- Going gluten- and dairy-free can be difficult, expensive and boring. When I’ve adhered to her advice, my joints are less achy, my nose has stopped running and I never get bloated. I’m working at making these changes work for me more often.
• INFLAMMATION – With the anti-inflammatories, I nap less and feel less groggy in the afternoon. I have normal blood panels regularly for the first time in my adult life. Whenever I had a complete blood count (CBC) I usually had at least one low value. This year I’ve had two normal CBC’s in a row. That’s a significant change for me. I’ll continue to monitor my CRP levels with my insurance covering providers.
• NUTRITION – With the supplements and a better diet, I don’t feel quite as depleted or thrown off when super-stressed.
• ENERGY – I found a therapist covered by my insurance who does tapping and energy work along with talk therapy. My spiritual needs are met by weekly yoga, hikes, the poetry of Mary Oliver and Rumi, connecting with other survivors of ACEs who “get it” so we can “get it together.” My almost daily practice of listening to guided meditations and imagery from healers such as Tara Brach, Cheri Huber, Pema Chodron, Belleruth Naparstek and Rick Hanson is most helpful. All validate the impact of grief, trauma and adversity and also offer relief – teaching why and how mindfulness-based approaches can be helpful.
• Although I switched from Paxil to Prozac -- something I’d failed to achieve prior to incorporating Vasile’s protocol -- I did not wean off all my medications as I’d hoped. As a single mother I couldn’t afford not to be fully functioning. I need to be emotionally present and to pay the bills.
From first-hand experiences, I know trauma-informed care can improve physical and emotional health. I wish it were available still to me and others with ACEs.
At least I know we ACE-informed patients can make a difference. Vasile now uses the 10-question ACE survey in her practice.
“We use the ACE score on our intake form,” she said.
It’s “so great to have this information when meeting with patients,” she said. “Clearly there’s so much more coming with them than their complaint at hand -- and so much more risk should we not be aware of their ACEs.”
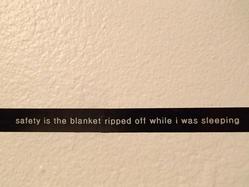
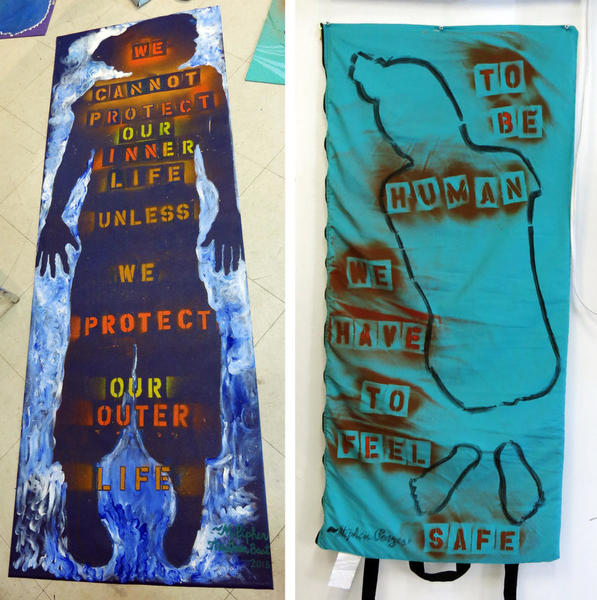
Note: ACE photos and art by Margaret Bellafiore and author as part of Body Language, as interactive installation at Mobius.













Comments (4)