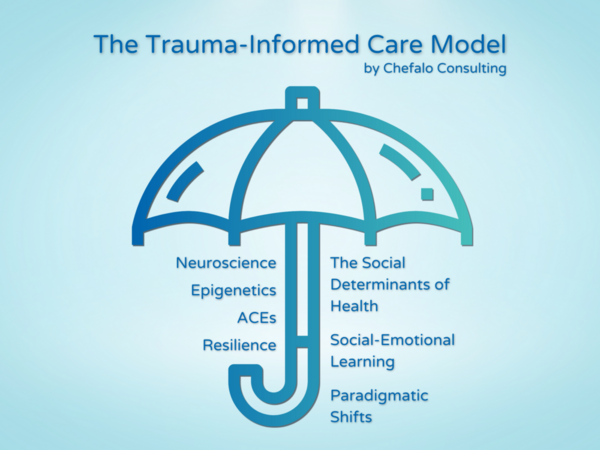
Trauma-informed care is like an umbrella that encompasses the social determinants of health, social-emotional learning, and actionable solutions to create real change. I think a lot of people don’t understand this yet.
Understandably, when people hear “trauma-informed,” they’re confused. If you’re not already informed about the impacts of and solutions to widespread trauma in our society, it’s hard to imagine what type of information relates to trauma.
So, let me frame it with language that you might be more familiar with: the social determinants of health and social-emotional learning.

What are the social determinants of health (SDOH)?
In circles that discuss trauma-informed care and the social determinants of health, I’ve noticed that a lot of people are confused as to how these two models intersect. A startling number of people assume that these models are completely distinct and share no common ground.
The opposite is true.
The social determinants of health (SDOH), social-emotional learning (SEL), and trauma-informed care (TIC) are all research-based models intended to improve outcomes for people, particularly disadvantaged individuals.
To give you a better idea of why the SDOH are important, consider this heartbreaking but insightful perspective from Laura Gottlieb:
“I had diagnosed ‘abdominal pain’ when the real problem was hunger […] I mislabeled the hopelessness of long-term unemployment as depression and the poverty that causes patients to miss pills or appointments as noncompliance. In one older patient, I mistook the inability to read for dementia. My medical training had not prepared me for this ambush of social circumstance. Real-life obstacles had an enormous impact on my patient's lives, but because I had neither the skills nor the resources for treating them, I ignored the social context of disease altogether.”
-Laura Gottlieb, The San Francisco Chronicle
Trauma-informed care provides the skills, resources, and training that professionals like Gottlieb need. And while TIC is often discussed in the public health sector, it is applicable to almost every other industry, too.
The US Department of Health and Human Services identifies five key domains within the social determinants of health:
1. Economic Stability
2. Education Access and Quality
3. Health Care Access and Quality
4. Neighborhood and Built Environment
5. Social and Community Context
The basic concept surrounding social determinants of health says that if you lack access and opportunity to certain things that significantly affect your quality of life (such as money, food, housing, healthcare, education, safety, family, etc.), your health will suffer.
The trauma-informed model agrees, but the language we use is a bit different. We refer to this lack of access and other negative experiences collectively as trauma.
What are adverse childhood experiences (ACE)?
ACEs are one key concept within the trauma-informed model, and there’s a lot of research to back up what we know about ACEs. And there’s more coming: the CDC is currently conducting the largest ACE study in history in partnership with Kaiser Permanente.
Some examples of ACEs include:
- Poverty, Homelessness, and Poor Housing Quality
- Lack of Opportunity, Economic Mobility, and Social Capital
- Experiencing or Witnessing Violence
- Mental Illness and Substance Abuse
- Physical & Emotional Neglect or Abuse
- Discrimination
- Incarceration
- Natural Disaster
If you want to calculate your ACE score and learn more about what we know about ACEs, check out this article that addresses why ACEs are a major public health concern.
Using the SDOH lens, we can see how these factors impact a person’s outcomes in life. The TIC model specifically names these as ACEs and/or trauma (what is traumatic for one person may not be traumatic for another—but this is a conversation for another day).
The challenges named within the key domains of the SDOH (economic stability, access to quality education and health care, neighborhood and built environment, and social/community context) become adverse childhood experiences when they are experienced in the early stages of life.

What is social-emotional learning (SEL)?
The Collaborative for Social Emotional Learning (CASEL) defines social-emotional learning as “an integral part of education and human development.”
SEL helps us:
- develop healthy identities
- make responsible and caring decisions
- manage our emotions
- feel and show empathy for others
- set and achieve personal & collective goals
- establish and maintain supportive relationships
Basically, social-emotional learning encompasses all the processes, skills, and techniques that we need to learn to achieve psychological or mental well-being. It relates to our ability to socialize, access our feelings, behave appropriately, and empower ourselves.
CASEL identifies five social and emotional learning core competencies
1. Self-Awareness
2. Self-Management
3. Social Awareness
4. Relationship Skills
5. Responsible Decision Making
Next week, we’ll get into the details of emotional intelligence (EI) and why EI is essential for trauma-informed leaders.
For now, you should know that trauma-informed care also teaches social-emotional skills, such as healthy communication, mindfulness, emotional regulation, and relationship-building, through a lens that acknowledges why trauma can create obstacles for us when learning and practicing these skills.
How do SDOH, SEL, and ACE relate to trauma-informed care?
These models have laid the groundwork for TIC. We all agree on the facts. The key difference is perspective.
Where others may see someone who struggles with SEL and say, “They need to do better. Why are they so difficult?”, the trauma-informed model sees someone who struggles and asks, “What has made this hard for them? Where can I see strengths?”
Trauma-informed care takes the SDOH and SEL a step further by applying paradigmatic shifts that push us to move from “What’s wrong with you?” to “What happened to you?” Then, we take it further to ask, “What’s strong in you?”
The value of trauma-informed care
The trauma-informed model can help anyone, anywhere, but it’s especially pertinent to social service providers.
Whether you work in healthcare, education, or the court system, your ultimate goal is to assist people in need, and these people are often high-risk individuals with a history of trauma. The trauma-informed model ensures that you don’t do more harm while trying to do good, which is why it is so essential.
If you work in any other sector, the trauma-informed model still has countless benefits, such as improved communication & collaboration, stronger teams, and a healthy workplace culture. All these cultural changes translate into measurable improvements, too, such as lower healthcare costs, reduced stress, and decreased turnover.
There are a lot of moving parts when it comes to the TIC model. If you want to learn more about how the trauma-informed framework can help you or your organization, you can book a free consultation with a trauma-informed expert.
Chefalo Consulting also hosts free, hour-long, trauma-informed networking sessions, where you can pop by to ask a quick question or listen in to learn more. New dates coming soon for our Intentional Conversations, so keep any eye on our website and the PACE's Connection Calendar very soon!





Comments (5)