What ACEs do you have?
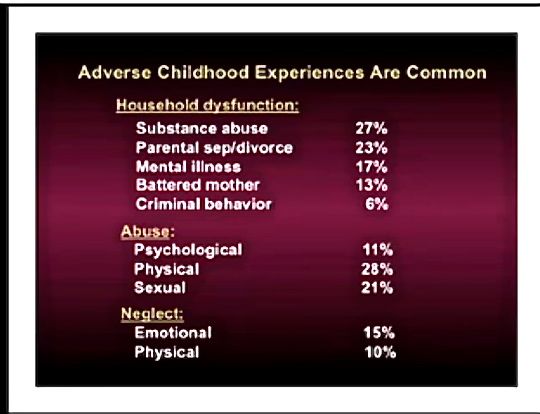
There are 10 types of childhood trauma measured in the CDC-Kaiser Permanente Adverse Childhood Experiences Study. (There are many others...see below.) Five are personal — physical abuse, verbal abuse, sexual abuse, physical neglect, and emotional neglect. Five are related to other family members: a parent who's an alcoholic, a mother who's a victim of domestic violence, a family member in jail, a family member diagnosed with a mental illness, and experiencing divorce of parents. Each type of trauma counts as one. So a person who's been physically abused, with one alcoholic parent, and a mother who was beaten up has an ACE score of three.
There are, of course, many other types of childhood trauma — racism, bullying, watching a sibling being abused, losing a caregiver (grandmother, mother, grandfather, etc.), homelessness, surviving and recovering from a severe accident, witnessing a father being abused by a mother, witnessing a grandmother abusing a father, involvement with the foster care system, involvement with the juvenile justice system, etc. The ACE Study included only those 10 childhood traumas because those were mentioned as most common by a group of about 300 Kaiser members; those traumas were also well studied individually in the research literature.
The most important thing to remember is that the ACE score is meant as a guideline: If you experienced other types of toxic stress over months or years, then those would likely increase your risk of health consequences, depending on the positive childhood experiences you had (see below).
Prior to your 18th birthday:
- Did a parent or other adult in the household often or very often… Swear at you, insult you, put you down, or humiliate you? or Act in a way that made you afraid that you might be physically hurt?
No___If Yes, enter 1 __ - Did a parent or other adult in the household often or very often… Push, grab, slap, or throw something at you? or Ever hit you so hard that you had marks or were injured?
No___If Yes, enter 1 __ - Did an adult or person at least 5 years older than you ever… Touch or fondle you or have you touch their body in a sexual way? or Attempt or actually have oral, anal, or vaginal intercourse with you?
No___If Yes, enter 1 __ - Did you often or very often feel that … No one in your family loved you or thought you were important or special? or Your family didn’t look out for each other, feel close to each other, or support each other?
No___If Yes, enter 1 __ - Did you often or very often feel that … You didn’t have enough to eat, had to wear dirty clothes, and had no one to protect you? or Your parents were too drunk or high to take care of you or take you to the doctor if you needed it?
No___If Yes, enter 1 __ - Were your parents ever separated or divorced?
No___If Yes, enter 1 __ - Was your mother or stepmother:
Often or very often pushed, grabbed, slapped, or had something thrown at her? or Sometimes, often, or very often kicked, bitten, hit with a fist, or hit with something hard? or Ever repeatedly hit over at least a few minutes or threatened with a gun or knife?
No___If Yes, enter 1 __ - Did you live with anyone who was a problem drinker or alcoholic, or who used street drugs?
No___If Yes, enter 1 __ - Was a household member depressed or mentally ill, or did a household member attempt suicide? No___If Yes, enter 1 __
- Did a household member go to prison?
No___If Yes, enter 1 __
Now add up your “Yes” answers: _ This is your ACE Score
__________________________
Now that you know your ACEs, what does it mean?
First....a tiny bit of background to help you figure this out.....(if you want the back story about the fascinating origins of the ACE Study, read The Adverse Childhood Experiences Study — the largest, most important public health study you never heard of — began in an obesity clinic.)
The CDC's Adverse Childhood Experiences Study (ACE Study) uncovered a stunning link between childhood trauma and the chronic diseases people develop as adults, as well as social and emotional problems. This includes heart disease, lung cancer, diabetes and many autoimmune diseases, as well as depression, violence, being a victim of violence, and suicide.
The first research results were published in 1998, followed by more than 70 other publications through 2015. They showed that:
- childhood trauma was very common, even in employed white middle-class, college-educated people with great health insurance;
- there was a direct link between childhood trauma and adult onset of chronic disease, as well as depression, suicide, being violent and a victim of violence;
- more types of trauma increased the risk of health, social and emotional problems.
- people usually experience more than one type of trauma – rarely is it only sex abuse or only verbal abuse.
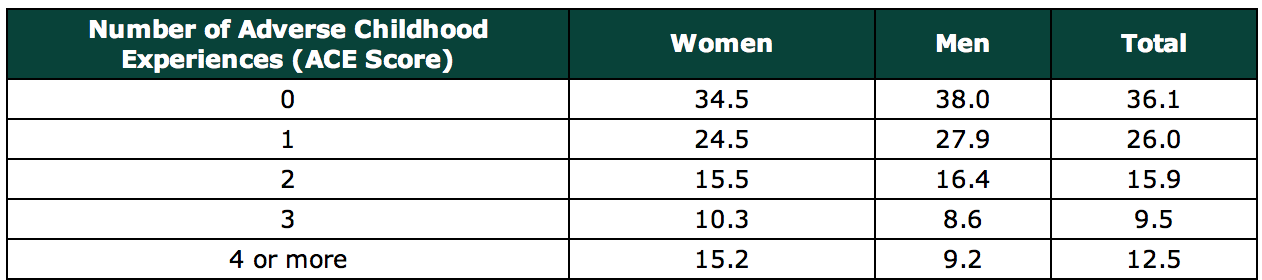
A whopping two thirds of the 17,000 people in the ACE Study had an ACE score of at least one -- 87 percent of those had more than one. Thirty-six states and the District of Columbia have done their own ACE surveys; their results are similar to the CDC's ACE Study.
The study's researchers came up with an ACE score to explain a person's risk for chronic disease. Think of it as a cholesterol score for childhood toxic stress. You get one point for each type of trauma. The higher your ACE score, the higher your risk of health and social problems. (Of course, other types of trauma exist that could contribute to an ACE score, so it is conceivable that people could have ACE scores higher than 10; however, the ACE Study measured only 10 types.)
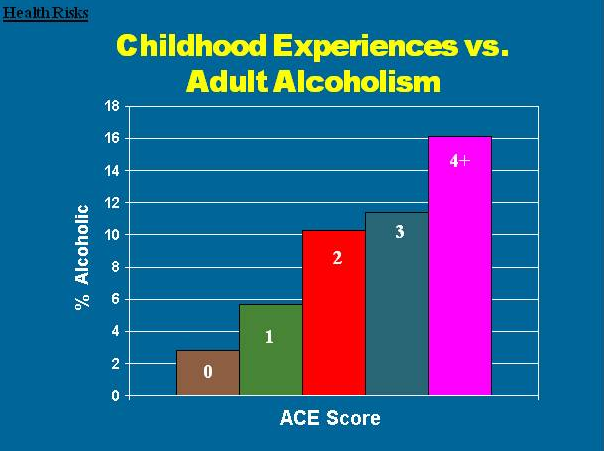
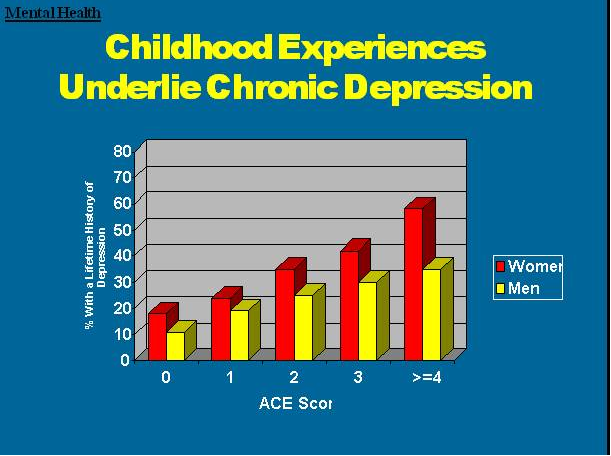
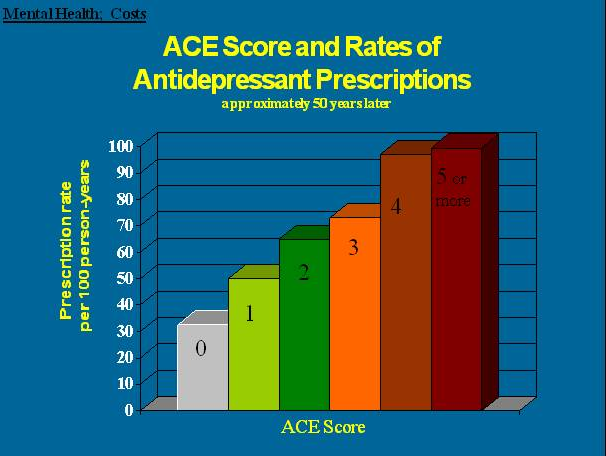
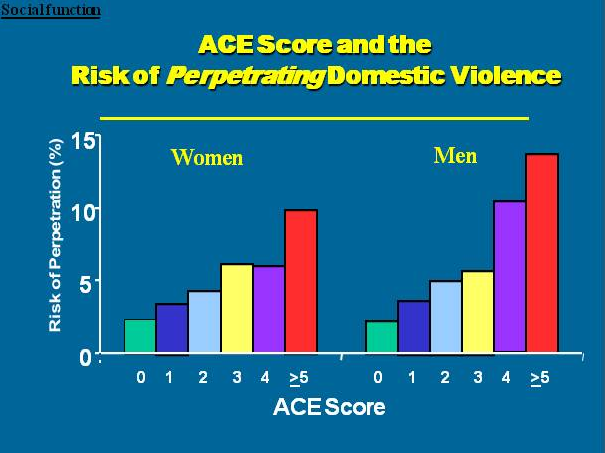
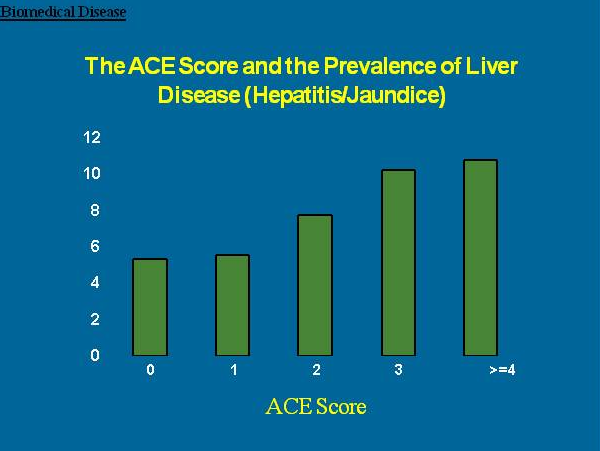
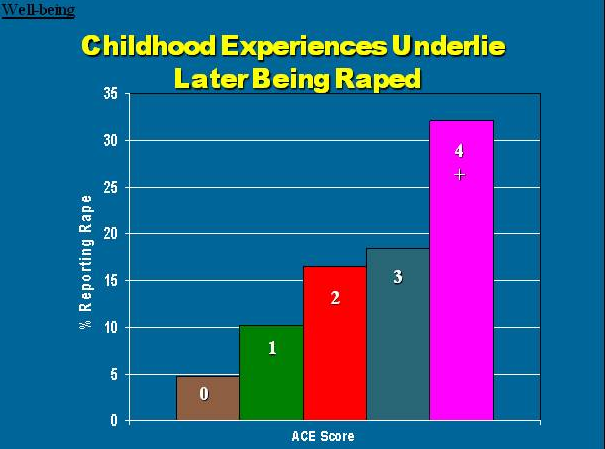
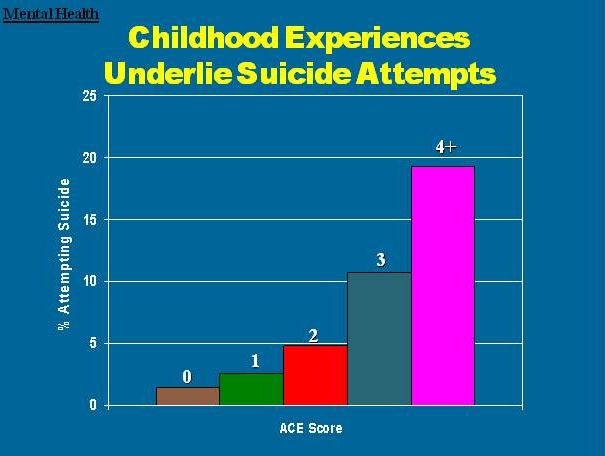
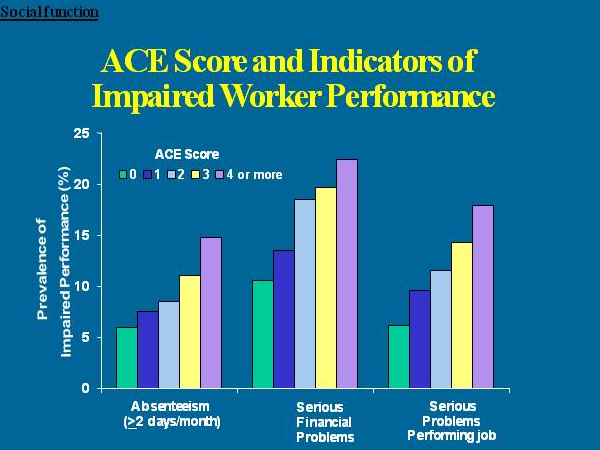
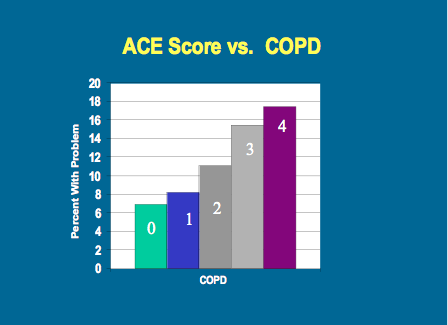
As your ACE score increases, so does the risk of disease, social and emotional problems. With an ACE score of 4 or more, things start getting serious. The likelihood of chronic pulmonary lung disease increases 390 percent; hepatitis, 240 percent; depression 460 percent; attempted suicide, 1,220 percent.
(By the way, lest you think that the ACE Study was yet another involving inner-city poor people of color, take note: The study's participants were 17,000 mostly white, middle and upper-middle class college-educated San Diegans with good jobs and great health care - they all belonged to the Kaiser Permanente health maintenance organization. Prior to the ACE Study, most research about effects of abuse, neglect, etc., involved poor people of color who live in the inner city. And so the notion was that it was inner-city people of color who experienced abuse, neglect, etc., not white middle-class or white upper-class people….that somehow white people of means were immune from the kinds of problems affecting people who were poor. That's not only ridiculous, but it was just another way to perpetrate racism and classism. The ACE Study quashed that notion. So, it’s not that I’m saying that the ACE Study is credible because it was done on white people, I’m saying that the ACE Study opened the door to an understanding that ACEs are at the root of nearly all problems of physical, mental, economic and social health in humans, no matter where in the world those humans live. The ACE Study and the other research that makes up ACEs science provided an opening to a better understanding of the constructs that make up our notion of why people suffer ill health — physical, mental, economic, social — and that includes systemic racism. )
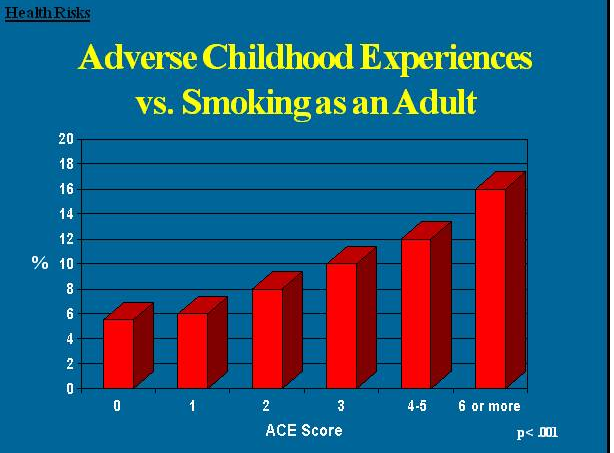
Here are some specific graphic examples of how increasing ACE scores increase the risk of some diseases, social and emotional problems. All of these graphs come from "The relationship of adverse childhood experiences to adult health, well being, social function and health care", a book chapter by Drs. Vincent Felitti and Robert Anda, co-founders of the ACE Study, in "The Hidden Epidemic: The Impact of Early Life Trauma on Health and Disease."
What causes this?
At the same time that the ACE Study was being done, parallel research on kids’ brains found that toxic stress damages the structure and function of a child’s developing brain. This was determined by a group of neuroscientists and pediatricians, including neuroscientist Martin Teicher and pediatrician Jack Shonkoff, both at Harvard University, neuroscientist Bruce McEwen at Rockefeller University, and child psychiatrist Bruce Perry at the Child Trauma Academy.
When children are overloaded with stress hormones, they’re in flight, fright or freeze mode. They can’t learn in school. They often have difficulty trusting adults or developing healthy relationships with peers (i.e., they become loners). To relieve their anxiety, depression, guilt, shame, and/or inability to focus, they turn to easily available biochemical solutions — nicotine, alcohol, marijuana, methamphetamine — or activities in which they can escape their problems — high-risk sports, proliferation of sex partners, and work/over-achievement. (e.g. Nicotine reduces anger, increases focus and relieves depression. Alcohol relieves stress.)
In addition, toxic stress can be passed down from generation to generation. The field of epigenetics shows that we are born with a set of genes that can be turned on and off, depending on what’s happening in our environment. If a child grows up with an overload of toxic stress, their stress-response genes are likely to be activated so that they are easily triggered by stressful situations that don’t affect those who don’t grow up with toxic stress. They can pass that response onto their children.
Fortunately, brains and lives are somewhat plastic. Resilience research shows that the appropriate integration of resilience factors — such as asking for help, developing trusting relationships, forming a positive attitude, listening to feelings — can help people improve their lives.
For more information about ACEs science and how it’s being used, go to: PACEs Science 101.
Here's a link to the long questionnaire (200+ questions).
For more information about PACEs science, go to PACEs Science 101.
_______________________
What are PCEs — positive childhood experiences?
Although there is still much to learn about ACEs and how to prevent and mitigate their effects, we also all know that childhood experiences are not limited to those that involve adversity. All childhood experiences matter. In the last few years, researchers have started to examine the impacts of positive childhood experiences (PCEs) on children and adults.
In 2019, a team of researchers — Dr. Christina Bethell, Jennifer Jones, Dr. Narangerel Gombojav, Dr. Jeff Linkenbach and Dr. Robert Sege — found a dose-response association between positive childhood experiences and adult mental and relationship health among adults who had experienced ACEs, irrespective of how many ACEs they had. This means that it's really important to have positive childhood experiences, no matter how much adversity you have in your life. And if you have a lot of adversity and a lot of positive childhood experiences, you are less likely to suffer the consequences of ACEs. However if you have no positive childhood experiences and few ACEs, the consequences of the ACEs are more likely to appear. Positive Childhood Experiences and Adult Mental and Relational Health in a Statewide Sample: Associations Across Adverse Childhood Experiences Levels | JAMA Pediatrics.
To find out what positive childhood experiences you have, answer the following questions. How much or how often during your childhood did you:
- feel able to talk to your family about feelings;
- feel your family stood by you during difficult times;
- enjoy participating in community traditions;
- feel a sense of belonging in high school;
- feel supported by friends;
- have at least two non-parent adults who took genuine interest in you; and
- feel safe and protected by an adult in your home.
- Also in 2019, Bethell, Gombojav, and Dr. Robert Whitaker reported that at each level of ACEs, “the presence of flourishing increased in a graded fashion with increasing levels of family resilience and connection.” Family Resilience And Connection Promote Flourishing Among US Children, Even Amid Adversity | Health Affairs
- In 2014, Bethell, Dr. Paul Newacheck, Dr. Eva Hawes, and Dr. Neal Halfon found that children with higher ACE scores were less likely to demonstrate resilience, live in a protective home environment, have a mother who was healthy, and live in safe and supportive neighborhoods. However, almost half of the children who had experienced ACEs also demonstrated resilience, and “resilience mitigated the impact of adverse childhood experiences on grade repetition and school engagement.” Adverse Childhood Experiences: Assessing The Impact On Health And School Engagement And The Mitigating Role Of Resilience | Health Affairs
- In a study published in 2021, Whitaker, Dr. Tracy Dearth-Wesley, and Dr. Allison Herman wrote that “greater childhood family connection was associated with greater flourishing in US adults across levels of childhood adversity.” Childhood family connection and adult flourishing: associations across levels of childhood adversity - Academic Pediatrics (academicpedsjnl.net)
- Dr. Yui Yamaoka and Dr. David Bard reported in 2019 that “the number of adverse childhood experiences was associated with both social-emotional deficits and developmental delay risks in early childhood; however, positive parenting practices demonstrated robust protective effects independent of the number of adverse childhood experiences.” Positive Parenting Matters in the Face of Early Adversity - PubMed (nih.gov)
- Among juvenile offenders, Dr. Michael Baglivio and Dr. Kevin Wolff discovered in 2020 that “high ACE scores were associated with increased reoffending, and high PCE scores were associated with decreased recidivism, as measured by both rearrest and reconviction. Further, among juveniles with four or more ACEs who have six or more PCEs, reconviction was 23% lower and rearrest 22% lower when compared to those youth with four or more ACEs and less than six PCEs, controlling for a host of demographic and criminal history measures.” Positive Childhood Experiences (PCE): Cumulative Resiliency in the Face of Adverse Childhood Experiences - Michael T. Baglivio, Kevin T. Wolff, 2021 (sagepub.com)
- Dr. Michael Baxter, Dr. Eden Hemming, Dr. Heather McIntosh, and Dr. Chan Hellman published research in 2017 that demonstrated that higher ACEs scores were associated with lower hope in a study of caregivers who brought children in for a child abuse medical investigation at a child advocacy center. Exploring the Relationship Between Adverse Childhood Experiences and Hope: Journal of Child Sexual Abuse: Vol 26, No 8 (tandfonline.com)
- In 2019, Dr. AliceAnn Crandall, Dr. Jacob Miller, Dr. Aaron Cheung, Dr. Lynneth Novilla, Dr. Rozalyn Glade, Dr. M. Lelinneth Novilla, Dr. Brianna Magnusson, Dr. Barbara Leavitt, Dr. Michael Barnes, and Dr. Carl Hanson observed in a study of adults that “higher counter-ACEs scores [i.e., positive childhood experiences] were associated with improved adult health and that counter-ACEs neutralized the negative impact of ACEs on adult health.” ACEs and counter-ACEs: How positive and negative childhood experiences influence adult health - ScienceDirect
- A study by Whitaker, Dearth-Wesley, and Herman in 2020 showed that across levels of childhood adversity, greater childhood family connection was associated with greater flourishing among young adults with type 1 diabetes.Childhood Family Connection With Flourishing in Young Adulthood Among Those With Type 1 Diabetes | Pediatrics | JAMA Network Open | JAMA Network
- Finally, in 2016, Bethell, Gombojav, Dr. Michele Solloway, and Dr. Lawrence Wissow examined ACEs, resilience, family protective factors, and emotional, mental or behavioral conditions (EMB) in children and youth in the U.S. The authors found that children with ACEs had higher EMB than children without ACEs, but the presence of resilience was significantly associated with lower amounts of EMB for both children with and without ACEs. In addition, the prevalence of EMB was lower when family protective factors were present, even if the child had ACEs, although the presence of two or more ACEs decreased the effect. Adverse Childhood Experiences, Resilience and Mindfulness-Based Approaches: Common Denominator Issues for Children with Emotional, Mental, or Behavioral Problems (nih.gov)
In terms of research, these are still early days, says Dr. Robert Whitaker, director of Research and Research Education at the Columbia-Bassett Program and professor of Clinical Pediatrics in the Vagelos College of Physicians and Surgeons at Columbia University: “This area of PACEs research is emerging, but the boundaries of that research have not really been defined, particular as complement to the well-established body of research on resilience.”
From “Brains: Journey to Resilience”, Alberta Family Wellness Initiative.
“PCEs may have lifelong consequences for mental and relational health despite co-occurring adversities such as ACEs,” noted Dr. Christina Bethell in Positive Childhood Experiences and Adult Mental and Relational Health in a Statewide Sample: Associations Across Adverse Childhood Experiences Levels. Bethell is professor at Johns Hopkins University in the Bloomberg School of Public Health and founding director of the Child and Adolescent Health Measurement Initiative. “In this way, they support application of the World Health Organization’s definition of health emphasizing that health is more than the absence of disease or adversity. The World Health Organization’s positive construct of health is aligned with the proactive promotion of positive experiences in childhood because they are foundational to optimal childhood development and adult flourishing.”
However, in terms of integrating what we know about PACEs, we have enough information to continue integrating the science into our work. If we want to change individuals, organizations, communities, and systems we need to talk about both positive and adverse childhood experiences — PACEs — and how they intertwine throughout our lives….
- At the individual level, learning about ACEs helps us understand why we behave the way we do, and that our coping behavior is normal…a normal response to abnormal circumstances. Learning about PCEs provides direction to heal. The key concept about PACEs is that learning about both, together, can help improve our health and well-being. It gives us hope.
- At the organizational level, staff and leaders can use knowledge of PACEs to create healing-centered work environments and programs in all sectors.
- At the community level, educating the public about PACEs can provide hope and foster the development of innovative ideas about how to support families, organizations and communities. Understanding the interplay between positive and adverse experiences offers opportunity for engagement with all sectors. Communities can use this new lens to create mindful, healing-centered, research-informed approaches to prevent adversity and encourage connection and healing.
- At the system level, policymakers and leaders can use research about PACEs to find common ground across fields and to support policies that promote the understanding of PACEs and how adversity and positive experiences work together.
At least two organizations are taking this approach and doing research to guide their actions:
- The Healthy Outcomes from Positive Experiences (HOPE) team at Tufts Medical Center have identified four building blocks that lessen the negative effects of ACEs: relationships, environments, engagement, and social emotional development. HOPE – Healthy Outcomes from Positive Experiences
- The Hope Research Center at the University of Oklahoma, Tulsa, focuses its research on the “science and power of hope as a psychological strength, especially among those experiencing trauma and adversity.” The Center defines hope as “the belief that the future will be better and you have the power to make it so.” Hope Research Center (ou.edu)




Comments (24)