As a primary care pediatrician, I spend most of my days talking about things that are hard for families. Parents ask what to do when their child won't poop on the potty. Or how to get their baby to sleep longer or how to get their teenager to wake up earlier. They ask how to get their child to sit in the car seat or what to do when they get car sick on long rides. And over the years I have developed a list of problem-solving strategies to help. But the one that has recently become my favorite is "how can I get her/him to stop having meltdowns?" because it leads me right to the heart of what most of my families really want help with.
Meltdowns were not what we spent a lot of time learning about in residency or medical school. I was taught to offer time-outs and 1,2,3 Magic. Time outs are falling out of favor and after decades of working with families, it is clear that these approaches often never "worked" and usually ended up with increased parental stress.
When I explore what is going on in these situations, parents are delighted to share what they tried, who suggested it and how they just don't know what else to do. Friends and family tell them they need to be stricter, to take more things and privileges away if their child continues to misbehave. But then they report how they just end up yelling and doing what their own parents did. Often these are things they experienced as traumatic when they were little and they have wanted, more than anything, not to recreate this for their children. But they end up doing it when things get hard.
I feel so grateful that parents bring these concerns to me, that my name is on their insurance card, so we can use these messy moments as a launching pad about how to talk about feelings and support each other through hard times. These messy moments allow us to help the family from perpetuating adversity to fostering resilience. We have to help them focus more on emotional wellness and self-care and less on behavior management. And this means we have to be comfortable talking about emotions and coaching families in healthy self-care strategies.
Parents crave this advice as much (if not more) than the advice we give about potty training or sleep problems. In the 2016 Zero to Three study (https://eric.ed.gov/?id=ED567804), parents of young children gave pediatricians a D- for the usefulness of our advice reporting it is as 62% effective. This is not because we don't mean well, it just is because our parenting advice doesn't usually include the most important part: what do you do when you tried to do what the doctor said and it didn't work.
Behavior problems are a precious opportunity to learn from our bad grades and make meaningful changes. We know from Bethell et al's 2019 study ( ) that positive childhood experiences (including being able to talk about your feelings with your family and feeling supported by your family during hard times) can offset the long term mental health impact of childhood adversity. And when I started figuring out how to support families with talking about feelings and supporting each other when things were hard, I started getting a much better report card for my parenting advice!
We can use these discussions about behavior problems to foster resilience while facilitating an increase children's PCE scores. Scores automatically go up at least by 2 when we help families talk about feelings which allows them then to support each other through hard times. But how do we do this? Again, this is not something we were taught in medical school or residency.
I have learned that these three steps are incredibly simple yet powerful:
1. First, families need to hear from professionals that it is okay that things aren't okay at home. We need to welcome the discussion about how things might be super messy at home or that they weren't actually able to use the advice we gave them before. Be curious. Ask about what it looked like when they tried to eat at the table as a family or limit screen time or start an exercise routine.
2. Next, we need to be able to support parents and children with problem solving about how to focus on everyone's emotions (which lead to the meltdown) rather than the behaviors or the meltdown itself. These can be very simple strategies such as singing a favorite song or belly breathing. With this approach, emotions are addressed as they arise with healthy coping strategies and fewer unmanageable emotions lead to what I affectionately call "screech." Mom sings the ABC song with her toddler who gets frustrated when he has to put away his toys so there's no clean up meltdown. Then as they get ready for nap time, mom models big deep belly breathing and there's no nap related meltdown.
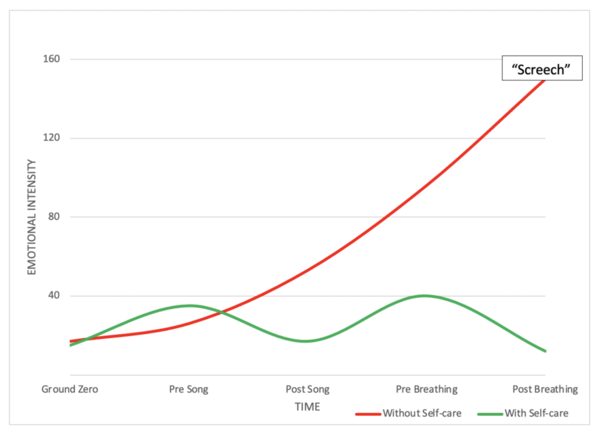
3. And finally, we have to help parents with their own stress level in real, accessible ways. While it's great to encourage parents to ask for help if they feel overwhelmed, what if next time they feel overwhelmed, they don't have anyone who can help them? Then they just feel more stressed and like they failed again. Parents can internalize the same self-care strategies we are suggesting for the children and can use breathing, singing, meditation or mindfulness.
If we really want to lower the impact of ACEs we have to do more than identify PCEs and celebrate when they are there. We have to roll up our sleeves and work with families on how to remove barriers when PCEs are not present. Talking about feelings and supporting each other through hard times requires us to know how to help parents learn to care for themselves when things are hard so they can do this for their children.
I teach parents and their kids to try pausing to take 5 big deep breaths when things are feeling hard. Even this short intervention is often enough for both parent and child to lower their stress levels.
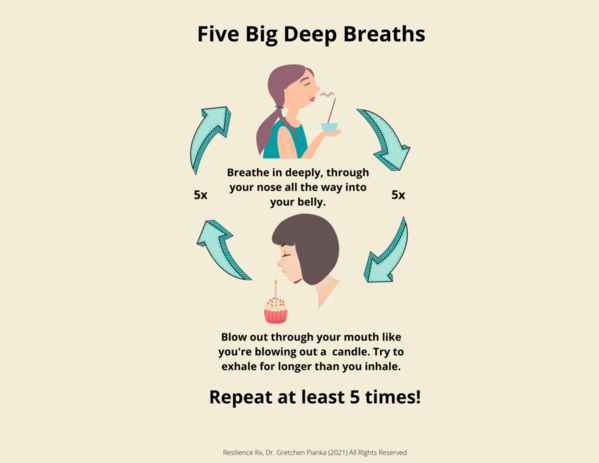
When stress is lowered, there is a better chance that at least one person's prefrontal cortex will be online and functioning and parents are more likely to be able to parent the way they intended!
We can start deploying stress-buffering strategies like this immediately. This simple approach is something we can do right away while we all continue to work as a society to prevent ACEs and establish a framework that allows more families to access the other things that have been proven to offset the long term mental health impact of adversity.


Comments (0)